Fungi or molds are the true ouroboros of nature.
After all, fungi eat illness and death, and in doing so, create new life.
I find the concept of fungi controlling the cycle of destruction and creation highly intriguing. I often ponder the biological processes that govern these laws of nature and their filamental connections to human beings.
In my capacity as a certified mold inspector and remediator based in the United States, I am well-versed in identifying mold (fungal) infestations in homes. These infestations often manifest as a specific odor reminiscent of decaying construction materials.
Repeated exposure to this distinctive scent has honed my detection skills over the span of a decade, allowing me to identify it with almost flawless accuracy.
The other day, it occurred to me: Wouldn’t humans with fungal infections or diseases produce a similar scent of decay or rot?
A brief online investigation confirmed my hypothesis!
Many studies have shown that humans demonstrate a proficient capacity to recognize and respond suitably to scent signals indicating danger such as certain chemicals resulting from biological decay processes to evoke avoidance (Rozin et al. 2000). Researchers have found that certain volatile compounds or smell hazards can be divided into two categories based on the human emotions associated with microbial threats (e.g., organic decay, vomit or feces) and nonmicrobial hazards (e.g., predators, fire, degraded air, and poisons).
For example, the smell of smoke would elicit fear that a fire is nearby and you need to move away or flee the area, while the smell of rotting garbage or moldy drywall will cause a disgusting emotion as the person inhales these VOCs. The reason is studies have shown that each class of threats is associated with a different underlying emotion such as disgust or fear/panic, which could indicate the level of threat.
This powerful smell detection system in animals and humans serves as an evolutionary defense mechanism deeply ingrained in our subconscious minds over millennia. The scents of decay, emanating as volatile compounds, serve as environmental cues for all living beings, including microorganisms, animals, and humans.
When we inhale, these odor molecules travel through the nasal passages and reach the olfactory epithelium, where they bind to the receptor proteins. This triggers a series of chemical signals that are sent to the brain, specifically the olfactory bulb, which processes and interprets the information to identify the scent.
While some scents signal the presence of food, others indicate potential threats such as predators, pathogens, fires, or even kin relationships.
Researchers have found that many individuals have reported experiencing a distinct change in their sense of smell when they or a loved one falls ill. This phenomenon is not merely coincidental; rather, it is rooted in the intricate connections between our olfactory system and our overall health.
I know this smell all too well.
When I was a young teen serving out my community service sentence in a senior citizen home, I could vividly remember this distinct smell as I walked down the lonely concrete halls.
This smell was not pleasant. It was a mixture of urine, feces, and rotting flesh.
As I served out my 30-day sentence, I felt every time I walked into that facility that I was walking on a narrow ridge between the shadow of the valley of death and life.
The next time I came across this unique scent again was in the ICU room of a hospital when my father had almost died from alcoholism at 52.
As I watched the nurses pump the shit out of his blood as he lay there incapacitated and near death because his liver gave out, that strange smell hit my nostrils bringing back memories of the nursing home.
Again, I realized where I was.
But this time I was a visitor witnessing my father’s life being dragged into the valley of death. As if they had, the legions received a notice of his impending doom coming to feast on his barely living carcass.
Today as I look back, I’m much more educated about human biology, health, disease, and death. As it relates to the scent of death, I have found an interesting correlation that explains this phenomenon.
What I found is that scent can be a powerful indicator of understanding the science of illness and death.
THE SCIENCE OF THE SMELL OF DISEASE
Our sense of smell, also known as olfaction, is a powerful and often underappreciated sense that plays a crucial role to detect and differentiate between a vast array of scents, from the pleasant aroma of freshly baked cookies to the pungent odor of rotten eggs and even infectious diseases.
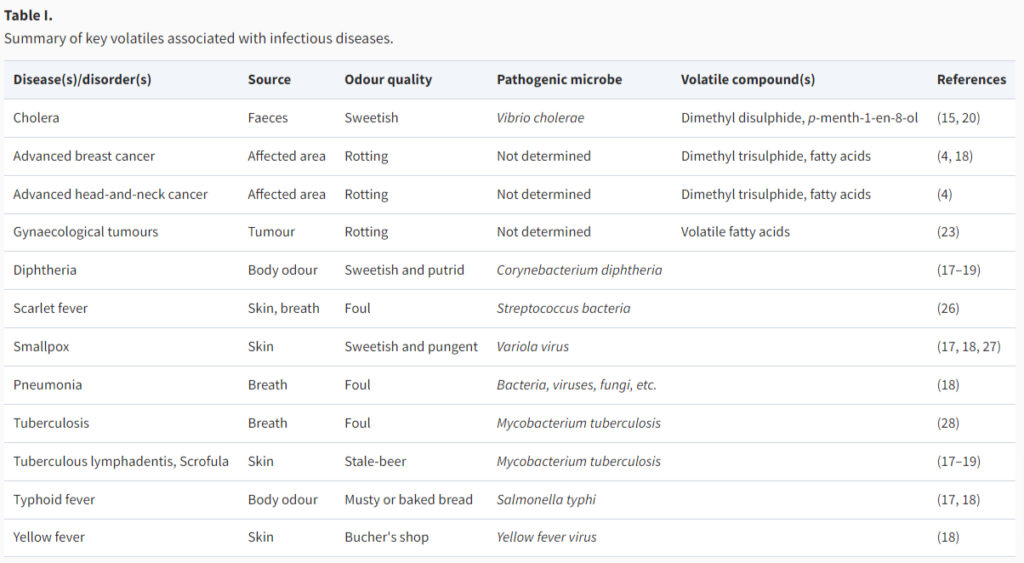
Clinicians have long recognized that most infections produce distinctive odors associated with a particular disease. In fact, each disease has a specific smell that is almost always associated with a rotten or decaying scent as if we are slowly being eaten alive, which appears to be the case.
In the human body, microbial organisms generate a variety of volatile substances, and different smelly compounds like alcohols, aliphatic acids, and terpenes. Research into the emission of VOCs resulting from microbial activity in bodily fluids and organs, which are then released through breath, urine, feces, and sweat traces back to the early 1800s.
The reason is that beyond exhaling air, your breath contains volatile compounds (VOCs) originating from various bodily organs that act as environmental signals (magnets) to nearby predators, pathogens, and kin.
If we have a fungal disease in one of our organs, they will emit these VOCs through our breath, sweat, skin, urine, feces, and vaginal secretions. But our blood is the most important source for these pheromone signals in the form of bodily odors.
For example, it’s common to experience morning breath, particularly if you’ve slept with your mouth open. However, bad breath or halitosis can also be a sign of underlying health issues such as gum disease, respiratory infections, or even digestive problems.
Persistent bad breath that doesn’t improve with regular oral hygiene measures like brushing and mouthwash could indicate an underlying issue such as infections in the sinuses, throat, or lungs, requiring medical attention from a healthcare professional.
When we smell these odors of other people, they are called pheremones which are small volatile organic molecules that animals and humans use to communicate. Pheromones are clinically defined as “substances which are secreted to the outside by an individual and received by a second individual of the same species, in which they release a specific reaction, for example, a definite behavior or a developmental process”.
Pheromones play a critical role in signaling and choreographing interactions between fungi mating partners during sexual reproduction.
Meaning, that certain smells give off a magnetic cue for fungi within the human body that they should start having lots of sex and reproduce more offspring, which would require that the increased fungal population needs more food to feast upon.
My theory is that this increased fungal load creates fermentation within our blood and organs which morphs this symbiotic relationship into a parasitic one leading to illness, disease, and eventually death. These illnesses caused by fermentation create a unique rot or decaying odor that we have the innate ability to detect.
Interestingly, I have found that research has revealed that certain illnesses can alter a person’s body odor, making them emit distinct pheromone scents that can be detected by others, even at a subconscious level. This ability to detect sickness through pheromones may have evolved as a survival mechanism, allowing us to avoid contact with individuals who are ill and reducing the risk of spreading disease within a community.
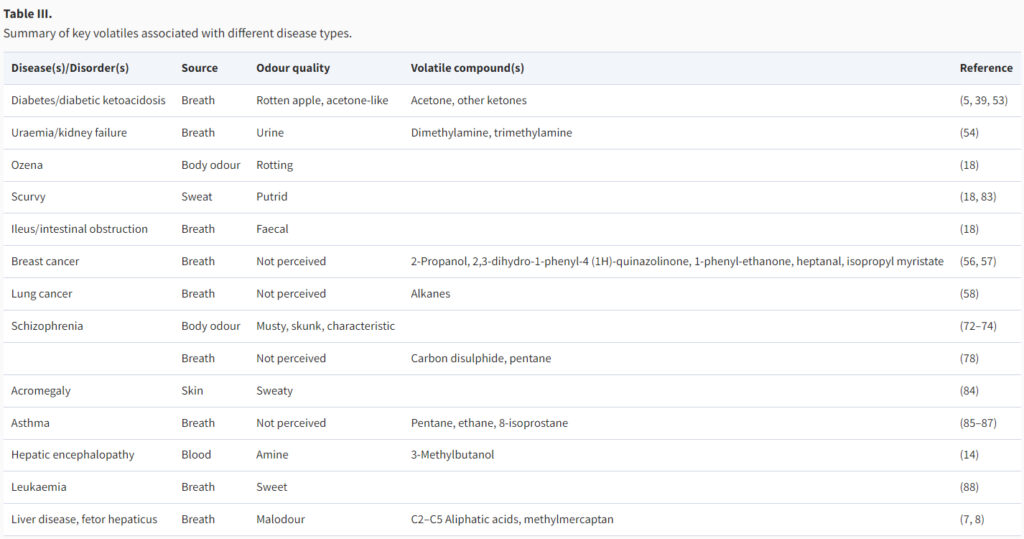
For example, researchers have found that certain infections like tuberculosis can create a unique odor in the patient’s sweat and even metabolic disorders such as phenylketonuria can result in a musty odor in the individual’s breath or skin. A fruity or rotten apple-like odor might indicate poorly controlled diabetes.
In some cases, organ failure can contribute to bad breath. Kidney failure, for instance, may produce an ammonia or urine-like odor, while serious liver disease can result in musty or garlic-like breath.
Another notable example is the use of scent analysis to detect early signs of certain types of cancer through breath samples. By analyzing the volatile organic compounds present in exhaled breath, researchers have been able to identify specific scent markers associated with different types of cancer, enabling early detection and intervention.
SMELL OF DEATH
Our olfactory senses have the remarkable ability to detect subtle changes in the body’s chemistry, even after passing. The unique scents that accompany different stages of decomposition can provide valuable insights into the time of passing and the processes at play within the body.
Before death, the human body undergoes a fascinating series of changes that can be detected through various senses, including smell. When a person is diseased or near death, the breakdown of cells and tissues initiates a complex biochemical process that releases volatile organic compounds (VOCs) into the surrounding environment. These VOCs are responsible for the unique pre and post-mortem scent that evolves.
Initially, the absence of vital functions such as circulation and respiration leads to a lack of oxygen supply to cells, resulting in anaerobic metabolism and the production of compounds like putrescine and cadaverine. These compounds contribute to the characteristic early-stage scent of death, often described as sweet and sickly.
As time progresses, microbial activity intensifies, causing further decomposition and the release of additional VOCs such as skatole and indole. These compounds give rise to the distinctive foul odor associated with the beginning stages of decomposition.
When a living organism ceases to function, a complex series of biological processes begin to unfold, leading to the breakdown of tissues and the release of various gasses and compounds.
The stages of decomposition can be broadly categorized into fresh, putrefaction, decay, and dry remains.
During the fresh stage, the body undergoes immediate changes such as algor mortis (cooling of the body), rigor mortis (stiffening of muscles), and livor mortis (discoloration of the skin due to pooling of blood). As the process progresses into putrefaction, bacteria within the body begin to break down tissues, releasing volatile organic compounds that contribute to the characteristic odors associated with decomposition.
Moving into the decay stage, the body continues to break down, leading to the formation of adipocere (a waxy substance) and further release of gasses such as methane and hydrogen sulfide. Finally, the remains enter the dry stage, characterized by the mummification of tissues and a reduction in odor production.
Studies have shown that as the body undergoes the process of decomposition, distinct scents are released that can provide valuable insights into the timeline of when an individual passed away.
One notable case study involved analyzing the volatile organic compounds (VOCs) emitted during decomposition. Researchers found that specific compounds, such as putrescine and cadaverine, increased in concentration over time, creating a unique scent profile associated with different stages of decomposition.
Health factors also play a crucial role in influencing post-mortem scent. Various health conditions and medications can impact the decomposition process and alter the odor profile after death. For example, individuals with certain illnesses may produce distinct chemical compounds during decomposition, leading to unique and identifiable post-mortem scents.
Researchers found that dying cells might signal their demise to nearby living cells by releasing specific metabolites, potentially orchestrating physiological responses to stress. Through mass spectrometry analysis of intracellular and extracellular metabolomes, they identified five metabolites involved in the process.
Additionally, they found adenosine triphosphate, previously known for its role in immune cell recruitment, to be upregulated after apoptosis induction. Importantly, the release of these metabolites was reduced when cells were treated with a pan-caspase inhibitor, suggesting that apoptotic cells actively release biologically relevant metabolites.
The authors explored whether metabolites released by dying cells were just incidental or reflect the cell’s activity before death. They found that spermidine levels were notably high in all models tested.
Spermidine is a naturally occurring polyamine that is present in various foods such as soybeans, wheat germ, and aged cheeses. In mammalian cells, spermidine is produced from putrescine, which is derived from ornithine, or through the oxidative breakdown of spermine.
It can also be taken up from the extracellular environment or expelled from the cell, potentially through membrane transporters akin to those found in yeast and bacteria, or through endocytosis/exocytosis mechanisms.
Spermidine is produced from putrescine.
A word that means “becoming putrid or rotting.”
This is the decomposition of carbon matter.
The scent of death.
Putrescine is found in all organisms and plants.
Its role is well documented to play a role in stress responses in plants and its absence is associated with an increase in both parasite and fungal populations in plants. It is what causes bad breath and vaginosis. Putrescine is found in semen and some microalgae, together with spermine and spermidine.
The intestinal microbiota represents the main source of spermidine synthesis within our body.
Studies of mice found that the concentration of spermidine in the gut lumen could be upregulated through oral administration of probiotics and the amino acid arginine, resulting in suppressed inflammation and improved longevity in old mice.
Due to its role in putrification, elevated putrescine has also been proposed as a biochemical marker for determining how long a corpse has been decomposing and also premortem diseases such as cancer. Scientifically speaking as it relates to humans, putrefying tissue of dead bodies breaks down our cells and proteins which undergo anaerobic splitting by bacteria and fungi creating a pungent scent that is emitted by putrescine.
Research on animals shows that it can function as a powerful chemosensory signal that prompts the perceiver to leave or avoid the area and that humans can identify threats via chemosignals. This unique scent has been studied to activate what is known as a “chemosensory warning signal” within humans activating threat management responses (e.g., heightened alertness, fight-or-flight responses).
The significance of scent in this realm cannot be understated, as it opens up a new dimension in forensic science that can lead to more accurate diagnosis, estimations, and conclusions in pre and post-mortem investigations.
Advancements in technology are paving the way for more accurate and efficient methods of determining illness, disease, and death based on scent analysis.
One promising development is the use of electronic nose devices, which are designed to mimic the human sense of smell and can detect and analyze volatile organic compounds (VOCs) emitted during decomposition. These devices have the potential to provide rapid and objective assessments of post-mortem scent profiles, aiding forensic investigators in determining the time of passing with greater precision.
Additionally, research is underway to explore the use of artificial intelligence and machine learning algorithms to analyze complex scent data patterns and identify specific biomarkers associated with different stages of decomposition.
CONCLUSION
Understanding the intricate relationship between the science of the scent of illness and death can pave the way for advancements in the diagnosis and prognosis of people infected by fungi.
Our olfactory system can serve as a powerful tool in identifying early signs of infectious disease, human decay, and organ rotting found in various diseases.
As we’ve explored in this article, clinicians have long recognized and several studies prove that many infections produce distinctive odors associated with particular diseases.
The sense of smell, often overlooked in healthcare settings today, will play a significant role in detecting and monitoring illnesses in the future.
By harnessing the power of our sense of smell, healthcare professionals can potentially improve early detection, treatment outcomes, and overall patient care.
The implications for humanity could be profound.
SOURCES:
PUBMED: Humans can detect axillary odor cues of an acute respiratory infection in others
Pheromones and their effect on women’s mood and sexuality – PUBMED
Spermidine: a physiological autophagy inducer acting as an anti-aging vitamin in humans?
The smell of death: evidence that putrescine elicits threat management mechanisms
An Initial Evaluation of the Functions of Human Olfaction

Moe is the founder of GnosticWarrior.com. He is a father, husband, author, martial arts black belt, and an expert in Gnosticism, the occult, and esotericism.



![How Coinred, king of the Mercians, and Offa, king of the East Saxons, ended their days at Rome, in the monastic habit; and of the life and death of Bishop Wilfrid [709 A. D.] | Book 5 | Chapter 18 How Coinred, king of the Mercians, and Offa, king of the East Saxons, ended their days at Rome, in the monastic habit; and of the life and death of Bishop Wilfrid [709 A. D.] | Book 5 | Chapter 18](https://www.gnosticwarrior.com/wp-content/plugins/contextual-related-posts/default.png)
